Parkinson's disease stems from the stomach? Studies have confirmed that pathogenic proteins crawl from the intestines into the brain
July 01, 2019 Source: Academic Jingwei WeChat public number
Window._bd_share_config={ "common":{ "bdSnsKey":{ },"bdText":"","bdMini":"2","bdMiniList":false,"bdPic":"","bdStyle":" 0","bdSize":"16"},"share":{ }};with(document)0[(getElementsByTagName('head')[0]||body).appendChild(createElement('script')) .src='http://bdimg.share.baidu.com/static/api/js/share.js?v=89860593.js?cdnversion='+~(-new Date()/36e5)];There is growing evidence that Parkinson's disease is not only a brain lesion, it is associated with the intestines. A research team at the Johns Hopkins University School of Medicine recently demonstrated that Parkinson's disease originates in the intestines, and that nerve-killing proteins pass from the intestines to the brain. The paper was published online in the authoritative academic journal Neuron. This work also provides a new model for the treatment of Parkinson's disease, which can be used to test for the prevention of disease and the prevention of deterioration.
The intestinal problem has long been a clue?
200 years ago, a surgeon named James Parkinson reported a "irritating and painful disease" that was named "tremor palsy" based on the patient's most prominent symptoms.
At the same time, Dr. Parkinson noted that these patients have suffered from constipation. In addition, one of the six cases he described appears to have reduced exercise-related problems after taking medications for the gastrointestinal tract. The role of the intestine in Parkinson's disease may have been laid down when people first recognized the disease.
Today's doctors also notice that constipation is one of the most common symptoms of Parkinson's disease and often occurs earlier than the onset of dyskinesia.
However, past research and treatment of Parkinson's disease has focused on the brain.
Scientists have found that the brains of patients with Parkinson's disease have a characteristic: a protein called α-synuclein (α-syn) is abnormal, and misfolded proteins are accumulated in the brain. , leading to the death of nerve cells in the relevant parts. For example, in the substantia nigra of the brain, the death of neurons that produce dopamine reduces the dopamine, a key neurotransmitter that regulates motor and mood functions.
In 2003, when the German neuroanatomist Heiko Braak examined the autopsy results of patients with Parkinson's disease, he unexpectedly found that in addition to the brain, the nervous system controlling the gastrointestinal tract also has accumulation of α-syn protein, and the appearance time corresponds to The early stages of disease development. Therefore, Professor Braak had boldly speculated that perhaps Parkinson's disease originated in the intestines?
However, is protein deposition in the patient's intestinal nervous system the same as protein deposition in the brain that kills neurons? If it is the same thing, how do they go from the intestines to the brain? Will Parkinson's disease invade the brain along the nerves that connect the intestines and brain like ladders? There was no evidence at the time.
"cable" from the intestines to the brain
In this new study, neuroscientist Professor Ted Dawson led the research team to create a novel animal model to answer the above questions, and finally provided the hypothesis that Professor Parkinson's disease originated from the stomach after Professor Braak made the hypothesis more than ten years later. Experimental evidence.

Professor Ted Dawson, co-author of the study, is a well-known expert in the field of neurodegenerative diseases (Source: Johns Hopkins University School of Medicine)
The team injected the synthetic pathological alpha-syn protein into the gastrointestinal muscles of dozens of healthy mice. At 1 month, 3 months, 7 months, and 10 months after the injection, they sampled and analyzed the brain tissue of the mice.
The results showed that after 1 month of injection, the pathological α-syn protein had spread to the brainstem at the base of the brain; at 3 months, it spread upward to the blue and black matter, and even reached the amygdala, hypothalamus and forehead. Leaves; by 7 months, spread to more brain areas, including the hippocampus, striatum and olfactory bulb. The process of spread is in line with the pathological development observed by Professor Braak in the brains of human Parkinson's disease patients!
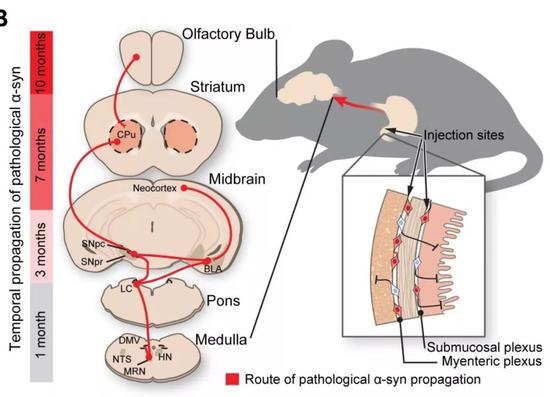
Misfolded α-syn proteins diffuse in the central nervous system at different stages after injection (Source: Reference [1])
In addition, after 7 months of injection, with the spread of pathological proteins to the striatum, brain imaging techniques showed a significant reduction in the production of dopamine in the brain of mice, which is also important for patients with Parkinson's disease. Pathological features.
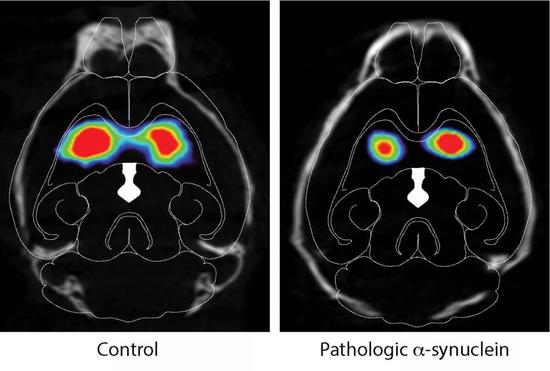
Brain imaging showed that the dopamine system in the brain of mice was damaged after injection of pathological proteins into the gastrointestinal tract (Source: Reference [1])
According to Professor Braak's observations and hypotheses, Parkinson's disease spreads from the gastrointestinal tract to the brain, and the vagus nerve may be an important pathway. The vagus nerve is emitted from the brainstem at the bottom of the brain, which dominates the main organs of the body, including the gastrointestinal tract.
The misfolded α-syn protein goes from the intestine to the brain. Is this cable channel going? To test this, the researchers did another set of experiments.
The same was true for the injection of pathological alpha-syn protein, but this time they surgically cut off the vagus nerve of the mouse. After 7 months, there were no signs of nerve cell killing in the brains of these mice. In other words, the cut nerve seems to prevent the progression of the pathogenic protein.
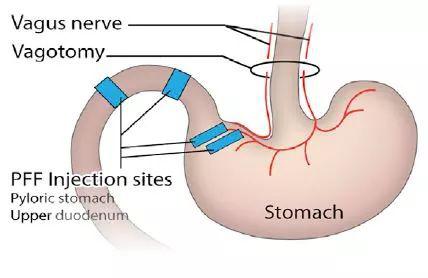
Schematic diagram of injection of protein and vagus nerve cut, the research team optimized the injection site and injection volume of the protein (Source: Reference [1])
Subsequently, the researchers further examined whether these physiological changes would lead to behavioral changes in animals. To do this, they let the mice accomplish two tasks: nesting and exploring new environments.
Nesting requires delicate and dexterous movements. For mice that had been injected with pathological proteins seven months ago, the task became difficult, and the nests they made were small and chaotic. "Like the symptoms of Parkinson's disease in humans, the ability to control fine motor movements deteriorates as the disease progresses," explains co-author Hanseok Ko.
In another task, mice with normal cognitive ability were curiously explored in the large box set up in the experiment, but mice affected by pathological proteins were very anxious and stayed at the edge of the box most of the time. This situation is also consistent with the symptoms of patients with Parkinson's disease.
In contrast, mice that cut off the vagus nerve and block the spread of pathological proteins performed similarly to normal mice without cognitive impairment.
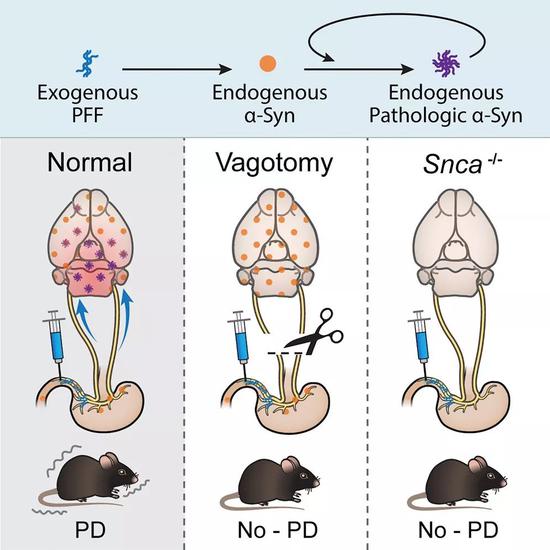
Schematic of the study (Source: Neuron)
Because the early and late-stage features, dyskinesia, and non-dysmotility associated with Parkinson's disease are reflected in mice, the team believes their results can provide new models for Parkinson's disease research, such as The effects of specific therapies are tested throughout the early stages of early symptoms to overall deterioration.
These results strongly support the hypothesis that Parkinson's disease originates from the intestines and reaches the brain. But Professor Ted Dawson sees farther. "First, this study will stimulate more research on future bowel-brain connections. Second, it is necessary to explore the factors, molecules, or causes of infection that cause misfolding and spread of alpha-syn proteins. Third, perhaps preventing the spread of alpha-syn protein from the intestine to the brain can be a target for treatment," he said.
We look forward to the constant exploration of scientists to bring effective treatments for the prevention and treatment of Parkinson's disease at an early date!
Source of the map: 123RF
Reference material
[1] Sangjune Kim et al. (2019) Transneuronal Propagation of Pathologic α-Synuclein from the Gut to the Brain Models Parkinson's Disease. Neuron. DOI: 10.1016/j.neuron.2019.05.035
[2] New mouse model of Parkinson's disease shows how it spreads from the gut. Retrieved Jun 27, 2019, from https://
[3] New research shows Parkinson's disease origins in the gut. Retrieved Jun 27, 2019, from https://
[4] Does Parkinson's Begin in the Gut? Retrieved Jun 27, 2019, from https://
[5] James Parkinson An Essay on the Shaking Palsy. Retrieved Jun 28, 2019 from https://neuro.psychiatryonline.org/doi/full/10.1176/jnp.14.2.223
Haida Equipment Service:
If you face any problems in future during testing process we promise we will give you a reply within 48 hours and solution provide within 3 working days. We can offer operation video and English operation muanual. We can provide video-con.
Onsite Service:
1.Device installation; 2.Equipment Operation Test Technology training;3.Equipment Calibration;4.Daily maintenance and maintenance of equipment
Free technical training for visiting factories
24-hour Online contact
Free software upgrades
Free information:
1.Product Instruction;2.Product operation instruction/video;3.Experiment Test (test application, test report)
Device Problem Handling:
1. Social media 24 hours online communication;2. Mail Seamless Docking;3. Video Conferencing;4. Artificial free door-to-door service
Salifert Test Kit,Aquarium Test Kit,Freshwater Test Kit,Fish Tank Test Strips
Changchun LYZ Technology Co., Ltd , https://www.lyzinstruments.com